The Health Index, titled Healthy States, Progressive India, published some time ago, presents an assessment of states and Union Territories, based on their health performance.
The second edition of the report was an outcome of NITI Aayog’s resolute optimism that a ranking exercise would encourage a competitive approach for potentially better outcomes, and would therefore be crucial for meeting sustainable development goals (SDGs). It takes the period 2017-18 as the reference year, and 2015-16 as the base year.
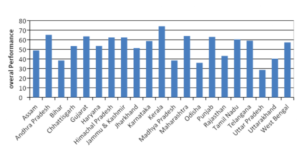
The Index evaluates the status of health in each state at two levels: overall performance and its incremental improvement.
Overall performance is an aggregate measure based on indicators in three domains: health outcomes, governance and key inputs and processes. It is judged on the basis of the composite index score, and accordingly categorises the states as ‘Front-runners’, ‘Achievers’ and ‘Aspirants’.
The incremental progress, on the other hand, is calculated as the change in composite Index scores as compared to the base year. It is thus an indication of the levels of momentum in states to realise health gains over the period from the base year to reference year.
There is significant variation in states’ overall performance. The composite index score of ‘Front runners’ is higher than 58.88, while that of ‘Aspirants’ has dwindled to below 43.74. The ‘Achievers’ hovered between 43.74 and 58.88.
The score for Kerala, ranked as the best performer for the second time, stands at 74.01, and Uttar Pradesh at the bottom end of the list has scored 28.61.
Andhra Pradesh (65.13), Maharashtra (63.99), Gujarat (63.52) and Punjab (63.01) are the other top performing states.
Together with Uttar Pradesh, Bihar (32.11), Odisha (35.97), Madhya Pradesh (38.39), and Uttarakhand (40.20) emerged as the least performing states.
There is wide disparity on the incremental progress too. States showing nil or even negative incremental change fared as ‘Not Improved’, those with 0.01 to 2.0 points increase as ‘Least Improved‘, an increase of 2.01 to 4.0 points marked them as ‘Moderately Improved’.
The ‘Most Improved’ ones reflected more than a four point increase. Among the larger states, twelve states displayed a positive incremental change in the Index score. But only seven out of these twelve states made significant incremental progress leading to improvement in the overall performance position.
Haryana was judged as the ‘Most Improved’ state as its health score increased the maximum, from 46.77 to 53.51. Rajasthan and Jharkhand too registered significantly high incremental performance.
Haryana qualified for this position not only on account of progress in most health outcome indicators like NMR (neonatal mortality rate), U5MR (Under 5 Mortality Rate), LBW (low birth weight in newborns) and SRB (sex ratio at birth), improvement in process related indicators too.
These indicators ascertained the proportionate size of vacant staff at the level of nurses, medical officers, institutional delivery, and the pace in which the fund flows from Centre to the spending unit. Bihar, on the other end, displayed the most negative incremental change.
Need to probe input and process indicators
The Index does a good job in providing a broad overview of performance of health services. The next step is an analysis of the areas highlighted in the report to examine the fundamental causes behind the problem.
As noted, the composite index discussed above is composed of 23 indicators, representing three domains – health outcomes, governance and information, key inputs and processes.
This article narrows down its focus on the sub components of the third domain, pertaining to key inputs and processes. Some important indicators of this domain include time taken for National Health Mission (NHM) funds to reach the implementation agencies, number of functional health facilities, proportion of vacant health care provider positions in public health facilities, like nurses, doctors, ANMs, specialists.
These indices need to be probed further to understand the causal factors resulting in deficits, and corresponding low scores for many states. There is a need to identify action areas for states, and apply the right strategies for improving their health outcomes. Only when each state takes this course for maximum incremental improvement, will the nation’s performance on health services go up.
Delays in fund flow
A Centrally-Sponsored Scheme cannot be implemented efficiently at the ground-level without ensuring that funds from the Centre reach the implementing agencies in a timely manner.
Data on the status of flow of Central NHM funds highlights huge dissimilarity in states (and UTs) in terms of the average number of days taken to transfer the fund from the Union level to Health Society responsible for expending these funds. A delay in fund transfer has a corresponding adverse effect on its utilisation.
Telangana has the most efficient system with the transfer happening on the same day. Bihar and Jharkhand are plagued by delays up to 191 and 187 days respectively.
Some others like Odisha, Madhya Pradesh, Tamil Nadu, and some smaller states like Tripura, Meghalaya and Mizoram are affecting the fund transfer relatively sooner.

Average number of days for transfer of Central NHM fund to implementing agency
NHM is governed by complex administrative procedures. An earlier study shows that the NHM budget has a break-up of over 1000 heads, with a very limited flexibility for utilising funds. The funds can be released by the state government only upon the issuance of a Sanction Order (SO).
This is a major factor contributing to the delays. Bottlenecks are also created by the fact that State Health Societies (SHSs) and the implementing agencies lie outside the administrative purview of the states.
Furthermore, the NHM budget has a break-up of over 1,000 heads, with a very limited flexibility for utilising funds, adding to the complicated architecture of fund release processes.
As a result, a high share of expenditure gets crowded in the last quarter of the financial year compounding the problem of low utilisation. Therefore, urgent efforts are needed to amend the rules and procedures that govern the release of public funds, with a focus to correct these systemic problems as a key strategy.
Conclusion
It is hoped that the findings of this report lead to more intense discussions on issues of fund flow delays across states, in the policy circles. Fund transfer delay, and associated complexity is an area most states need to focus on. Both the Centre and the States need to take steps to mainstream the sector by addressing these deficiencies.
Interestingly, states who have been investing in nutrition and primary health care have managed to fix the systemic deficiencies, and are the high scorers in the Index.Achieving the SDGs on health will be difficult without understanding the causal factors of cracks in health care system. It is high time that the government paid attention to these loopholes that have long impeded progress in such an important sphere.The impetus of the intensive process of bringing out the Health Index can be used to drive the nature of health services and kick start reforming institutional processes.

 3 October, 2019
3 October, 2019